Pelvic Organ Prolapse: Health, Help, Hope, and Healing
Pelvic organ prolapse (POP) has been on medical record for nearly 4000 years, dating back to the Kahun Gynaecologic Papyrus circa 1835 B.C., yet remains shrouded in stigmatized silence because of embarrassing symptoms. Women teens through end-of-life in every country around the world experience POP, yet seldom understand what is occurring in their bodies until after they are diagnosed with POP. It's long past time to talk out loud about the biggest secret in women’s health.
The pubococcygeus muscles (PC) are a trampoline-like set of muscles that sit at the base of the abdominal cavity, supporting the organs and structural tendons and ligaments above them. Pelvic organ prolapse occurs when the support structures above and below weaken and/or become damaged for a variety of reasons. One or more organs shift out of their normal positions, pushing into the walls of the vaginal canal, and eventually bulge outside of the vagina. There are 5 types of POP. Organs that can prolapse with POP are the bladder (cystocele), rectum (rectocele), intestines (enterocele), uterus (uterine), and vagina (vaginal vault). There are 4 levels of severity; grade 1 is the mildest, grade 4 the most severe.
Global Prevalence
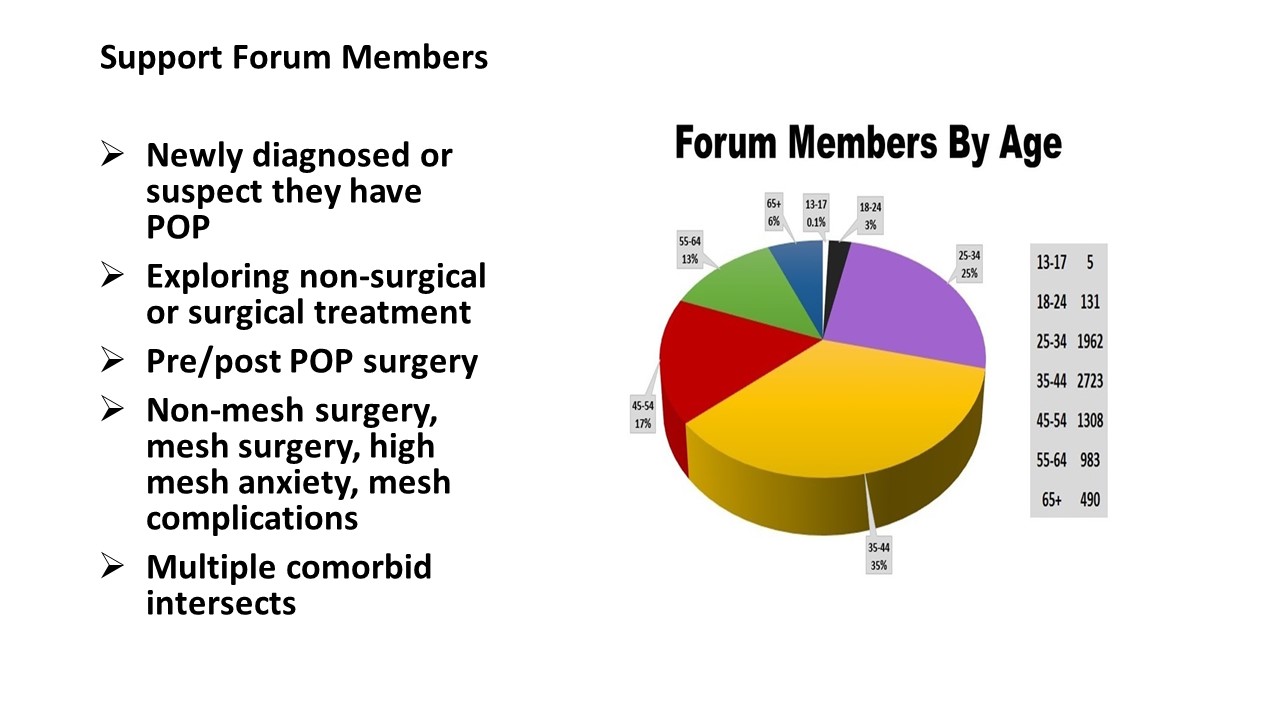
The current estimate for POP prevalence is 50% of 1 in 2 women will experience POP at some point in their life cycle. Accurate statistical capture for prevalence of pelvic organ prolapse in most countries is sorely lacking and difficult to estimate, because routine POP screening seldom takes place during standardized pelvic exams. Women experiencing POP may be too embarrassed to mention symptoms they are experiencing to their physicians; physicians unfortunately do not always ask the right questions, disabling appropriate diagnosis. POP is common in both developed and developing countries. APOPS currently has patient following in 183 countries. Within APOPS patient spaces, women from around the world clarify the physical, emotional, social, sexual, fitness, and employment quality-of-life impacts to women’s lives.
Statistics
Some current statistics related to pelvic organ prolapse are:
Research frequently estimates that up to 50% of women experience pelvic organ prolapse, but individual studies vary between 3-93% prevalence.
25-70% of women experience urinary incontinence. Stats vary significantly by study and incontinence type; not all UI is related to POP but UI is a common symptom of POP.
There are 300,000 surgeries annually in the US for POP.
Nearly 1/3 of women with pelvic organ prolapse will have multiple POP surgeries.
20% of women suffer sphincter damage during childbirth resulting in fecal incontinence.
In 2023, the majority of marathon participants identified as female (53.4%); 20-50% of women experience urinary leakage while exercising (running, jogging, aerobics), usually an indicator of a weak pelvic floor.
Research related to vaginal childbirth indicates that women are predisposed to the following types of damage that lead to pelvic organ prolapse:
Pressure on organs/tissues.
Pudendal nerve crush or stretch.
Levator Ani (pelvic floor muscle) denervation.
Levator Ani avulsion (tear)
Connective tissue damage (fascia).
Pelvic floor muscle weakening.
Mechanical disruption of rectal sphincter.
PELVIC ORGAN PROLAPSE Symptoms
Each of the 5 types of POP has its own symptoms, but in general the most common symptoms include:
Tissues bulging out of the vagina.
Pressure, pain, or ‘fullness’ in vagina or rectum or both.
Urinary incontinence.
Urine retention.
Fecal incontinence.
Chronic constipation.
Back/pelvic pain.
Tampons push out.
Painful intercourse.
Lack of sexual sensation.
Coital incontinence (leakage of urine or stool during intimacy).
PELVIC ORGAN PROLAPSE Causes
Vaginal childbirth and menopause are the 2 leading causes of pelvic organ prolapse, but there are multiple lifestyle, behavioral, and comorbid conditions that compound risk for all women. Females mid-teens through end-of-life experience POP. The most common causes of POP are:
Vaginal childbirth: complications from large birth weight babies, long 2nd stage labor, nerve damage, damage from forceps or suction deliveries, multiple childbirths, improperly repaired episiotomy. Impact of childbirth may occur immediately after a difficult delivery or may not show up until 20 years later. It is also possible for women who have never given birth to have POP; there are multiple non-childbirth related causes.
Menopause: age related loss of muscle tissue integrity is typically the result of a drop in estrogen level. Estrogen feeds muscle tissue, loss of estrogen in menopause impacts strength, elasticity, and density of muscle tissue.
Chronic constipation: a hernia in the colon (rectocele) is a leading cause of constipation in women. IBS (irritable bowel syndrome), poor diet, or lack of exercise may also impact regularity. Repetitively baring down to have a bowel movement pushes pelvic tissues downward. A rectocele can be both a cause and a symptom of POP.
Chronic coughing: smoking, allergies, bronchitis, and emphysema may cause chronic coughing which repetitively jerks tissues downward.
Heavy lifting: lifting children, employment related heavy lifting, fitness related weight lifting.
Hard foot-strike fitness activities: jogging, marathon running, aerobics, or gymnastics repetitively jerk internal structures downward.
Genetics: a family member with POP, especially mother/sister, may indicate an increased risk of POP. Ehlers-Danlos Syndrome also known as EDS (joint hypermobility, very stretchy skin) predisposes women to POP.
Neuromuscular disease: MS, Marfan (collagen deficiency).
Spina-bifida or stages of paralysis or wheelchair bound setting can predispose women to a weak pelvic floor; bladder exstophy (born with bladder outside the body) predisposes women to POP.
Diagnosis
The diagnostic process for pelvic organ prolapse will vary, based on the clinician you see and the tests he/she prefers to utilize. Gynecologists, primary care physicians, and other fields of practice providing pelvic exams can diagnose pelvic organ prolapse, but rarely have sufficient curriculum provided to determine type of POP or degree of severity accurately. Once diagnosed with POP, women are usually referred to a women’s health physio or a pelvic organ prolapse specialist, which are called Female Pelvic Medicine Reconstructive Surgeons (urogynecologists), and can be either a gynecologist or urologist. A POP subspecialist surgeon will provide a more definitive diagnosis and outline a path to successful treatment. Additionally, some cosmetic gynecologists treat pelvic organ prolapse. These specialists will be able to advise patients about both surgical and non-surgical treatment options. A POP specialist will typically perform the POP pelvic exam, and additional tests that may be required are:
Digital rectal exam.
Pelvic ultrasound or MRI.
Proctogram.
Urodynamic study.
Pelvic floor strength tests.
Hormone level evaluation.
Cystourethroscopy.
There are multiple surgical and nonsurgical treatment options for pelvic organ prolapse. The first step is to get a definitive diagnosis of type(s) and degree of severity of pelvic organ prolapse. Each treatment has unique benefits, and which choice you make will be influenced by your type of POP and grade of severity, lifestyle and behaviors, age, whether or not you are through having children, length of time you have been suffering with symptoms, intensity of symptoms, additional medical conditions, desire to have an active sex life, and financial or insurance considerations.
NON-SURGICAL PELVIC ORGAN PROLAPSE TREATMENTS
Often when women prefer non-surgical treatment, they are referred to physical therapists or physiotherapists. Women's Health physical therapists provide a significant variety of treatment options for POP. Since women's needs vary considerably based on type/degree of prolapse, treatment regimens will vary from woman to woman.
There are multiple non-surgical treatment options for POP; often women will utilize two or three treatment options at the same time for the best improvement of their symptoms. Non-surgical treatment options include:
Kegel Exercises.
Kegel assist devices.
Pessary.
Core/floor strengthening exercises.
Biofeedback.
Vaginal tissue regeneration therapy (laser or radio frequency).
Electrical Stimulation.
Hormone replacement therapy.
Support garments.
Tibial nerve stimulation.
Bulking agents.
There are multiple relatively new treatment options available to address specific symptoms of POP.
SURGICAL PELVIC ORGAN PROLAPSE TREATMENTS
There are multiple surgical treatment options for pelvic organ prolapse. once a definitive diagnosis is in place, you surgical choices will be outlined by your physician. Surgical treatment options include a variety of choices within each category; type utilized will vary with type/degree of POP and surgeon/patient preference:
Abdominal repair;
Transvaginal repair (through the vagina);
Robotic repair;
Laparoscopic repair;
Combinations of the above.
Urogynecologists have utilized polypropylene mesh for many pelvic organ prolapse procedures over the past years to provide a sustainable long-term repair. There has been considerable controversy regarding the use of polypropylene mesh for transvaginal procedures, and development continues to evolve based on country. Without the use of poly mesh, research indicates surgical repairs have a failure rate of approximately 30%. The specialists who treat POP may utilize synthetic, bio, or combination mesh repairs, native tissue repairs, or a combination of these procedures.
Impact to Intimacy
One aspect of pelvic organ prolapse that is significant and common is impact to intimacy. Coital incontinence (urine or stool leakage during intercourse), painful intercourse, or loss of intimate sensation can result in considerable relationship ramification. Open communication between partners is ideal, but seldom occurs when awkward POP symptoms occur. Spontaneity is difficult to achieve and POP symptoms can create a considerable roadblock to communication. Women may be too embarrassed to disclose symptoms to their partners, and men may assume women are not engaging in intimacy because they have no interest. When a medical condition is not disclosed to intimate partners, it creates boundaries that are difficult to overcome. When women are not aware of the cause of their symptoms and are too embarrassed to disclose details to their physicians, there can be a significant impact to a relationship.
Help and Hope for Women
Pelvic organ prolapse is a global women's health pandemic. POP undoubtedly encompasses the broadest demographic in women's health issues. Multiple types of pelvic organ prolapse display a variety of symptoms; women's unique childbirth, occupation, genetic, general health, and social activities vary significantly. The demographic variables are diverse. Countless women suffer silently with symptoms they don't understand. When we don't recognize the cause of symptoms, our minds can be our worst enemies, imagining the most negative scenario.
There is help and hope for women with POP. Treatment options evolve daily that can be utilized to control, improve, or repair this shrouded health condition. Women who have been diagnosed with POP need to come out of the closet with their diagnosis and treatment experiences and share information with their mothers, daughters, sisters, and friends. As pelvic organ prolapse becomes common knowledge for women, and routine screening for pelvic organ prolapse becomes an established aspect of routine pelvic exams, POP will become more recognized, acknowledged, and de-stigmatized, and women will be able to capture earlier diagnosis and treatment.
Additional POP links:
APOPS Energy
POP-Video