If you ask any 10 women how they feel about having a hysterectomy, you will likely get 10 completely unique responses, varying between a very strong interest in eliminating periods through horror at sacrificing what is felt to be the core of sexuality and/or femininity. While uterine-sparing surgical procedures are becoming more common to treat uterine prolapse (UP), hysterectomy continues to be the most commonly recommended surgical treatment. While some women reflect on how a hysterectomy will impact their sexuality, few realize it may impact their ability to have an orgasm, or the degree of orgasm intensity. Women experience two types of orgasm: external by means of clitoris stimulation or internal as a result of the thrust of a penis against the cervix within the vaginal canal. Women prefer to keep their orgasms intact and full-bodied regardless which type of orgasm they enjoy, thank you very much.
“Pelvic organ prolapse is seldom life-threatening,
but it is always life altering.”
Sherrie Palm
Though data varies by source, according to womenshealth.gov, every year in the United States roughly 400,000 women have hysterectomies, making it the second most common surgery among women in this country, following childbirth by cesarean delivery. But to what degree are sexual end results of hysterectomy explained to women prior to this procedure?
There are many reasons for hysterectomy, the majority of which are related to discomfort or quality of life issues such as:
Uterine prolapse.
Heavy periods that may or may not be caused by large fibroids.
Pelvic pain that may or may not be caused by endometriosis.
Unsuccessfully treated pelvic inflammatory disease (PID).
Adenomyosis, where the tissue that normally lines the uterus grows into the muscular wall of the uterus.
A minority of hysterectomies address life-threatening conditions, such as cancer, unmanageable infection, uncontrollable bleeding, or childbirth complications. Uterine prolapse is generally not considered a life-threatening, medically necessary reason for a hysterectomy, but UP absolutely has significant impact to quality of life. Generally, when women must decide whether to have a hysterectomy to treat uterine prolapse, sex is not at the top of the list of questions that get asked. The bigger concern tends to be a state of considerable discomfort, and the focus is making that discomfort disappear. Unfortunately, sexuality issues may crop up after the fact if they are not discussed prior to surgery.
Uterine prolapse is one of five types of pelvic organ prolapse. UP occurs when the uterus (womb) shifts from its normal position downward into the vaginal canal. The uterus may reposition partially into the vaginal canal, be completely positioned within the vagina, or may bulge outside of the vagina. Procidentia is the medical term used when the uterus has shifted completely beyond the outer edge of the vagina. Symptoms of uterine prolapse may include:
Vaginal pressure.
Pain with intercourse.
Irritation of cervix or uterine tissue bulging outside of the vagina from friction of the organ rubbing on undergarments.
Pain in lower abdomen or hip.
Feeling of vaginal fullness.
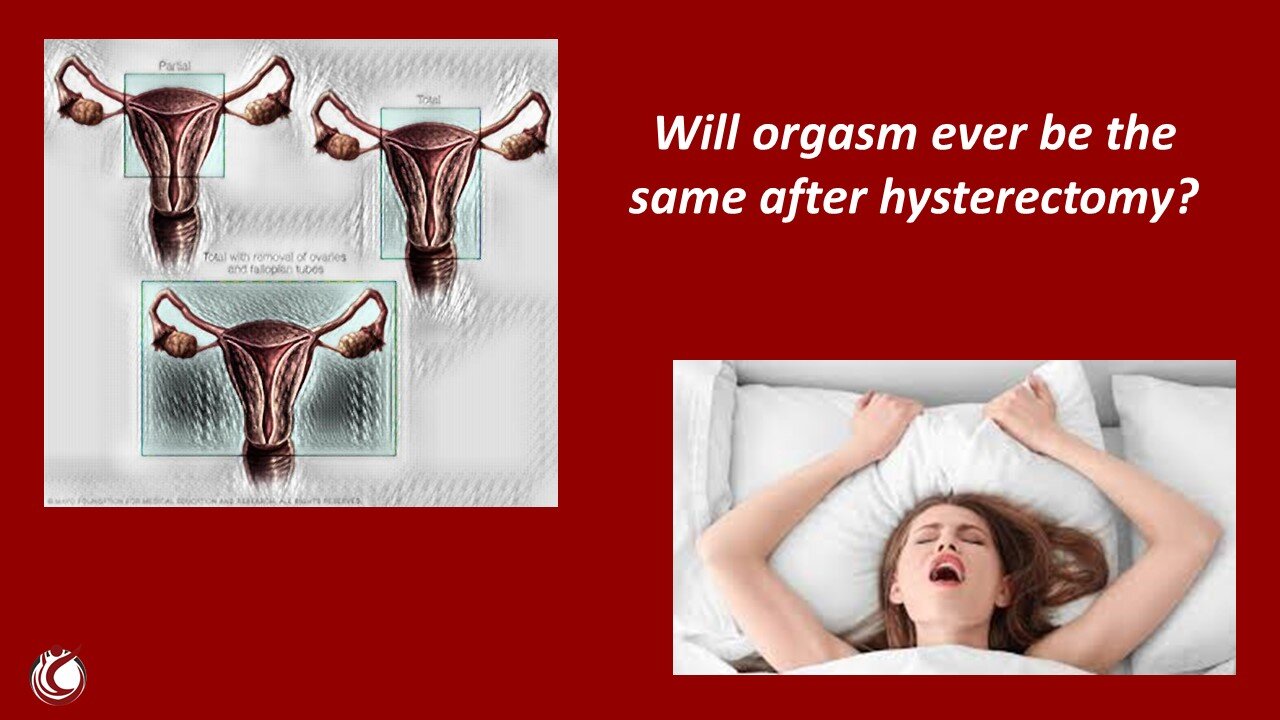
The type of hysterectomy a surgeon recommends will depend on the individual issues a woman is experiencing, such as co-existing medical conditions, the degree of severity of condition being experienced, and whether the condition is life-threatening. There are several types of hysterectomies:
Partial, where the uterus is removed but the cervix remains intact, (supracervical hysterectomy). A partial hysterectomy may also include oophorectomy, removal of ovaries and/or fallopian tubes. Removal of ovaries in a woman who is pre-menopausal will shift a woman into menopause. If a woman is post-menopausal, ovary removal will not reboot menopausal symptoms.
Total, removing the entire uterus including the cervix but leaving ovaries and fallopian tubes.
Total with oophorectomy, removing entire uterus with cervix as well as ovaries and fallopian tubes.
Radical (for cancer of uterus, fallopian tubes or ovaries) includes removal of the uterus, cervix, ovaries, fallopian tubes, possibly upper portions of the vagina and affected lymph glands, and fibrous and fatty connective tissue.
The technique a surgeon will choose varies based on their procedure of choice and patient needs. Types of surgical procedures for hysterectomy include:
Abdominal.
Vaginal.
Laparoscopic, with or without robot assist.
Robotic.
Additionally, some surgeons will offer a uterine-sparing procedure if it is an appropriate fit for the patient.
Complications or issues that may occur with or following a hysterectomy include:
Nerve damage, including loss of intimate sensation.
Vaginal shortening with vaginal route of repair.
Enterocele (small intestine drops into the space where the uterus was located or between the back vaginal wall and colon).
Vaginal vault prolapse (top of the vagina caves in on itself if structural support at the apex, the top of the vagina, is not secured during hysterectomy).
The generic phrase “you do not need your uterus” can and should engender questions from women, given the possible impact a hysterectomy may have to sexual sensation. Significantly, desire, arousal, or orgasm disorders may or may not occur post hysterectomy for UP. Some women experience a loss of intimate sensation, reduced ability to orgasm, or reduced orgasmic intensity. Additionally, the resulting shift in intimacy may affect self-esteem or body image. Research indicates both loss of sexual sensation and orgasmic reduction are related to nerve sever and/or loss of uterine contractions related to organ removal. While some women experience a loss of internal orgasm, they may still experience a clitoral orgasm, but sometimes the intensity of sensation may decrease. However, other women find that intimacy and sexual sensation improve, related to elimination of POP symptoms, such as pain, pressure, organ displacement, or nerve crush.
Ob/Gyn Suny Caminero, MD, and urogynecologist Stephanie Molden, MD, were kind enough to clarify in a bit more detail the impact of hysterectomy to intimate sensation. Below are their responses to the following questions:
How in depth are gynes and/or subspecialists educated regarding clitoral, vaginal, and cervical nerve-sparing tactics during hysterectomy?
Would there be benefit in a surgeon asking a woman whether her orgasms are clitoral or thrust/cervix/uterine related prior to surgery, or would this not have any impact on procedure chosen?
In women who have had a complete hysterectomy who have experienced considerable loss of capacity to orgasm, will any of the nonsurgical tools available have benefit to restore sensation to orgasmic level if a woman was previously able to orgasm?
Suny Caminero, MD: “Great questions and such an important topic. Before I answer, I’ll tell you my experience. I had a laparoscopic supracervical hysterectomy at 41 because of persistent bleeding and I was tired of pills, IUD’s and just the period in general. I am too busy to worry about my period. My sex life is 100x better after the hysterectomy and no loss of orgasm intensity. More orgasms now that I am not self-conscious about spotting or bleeding.
Now to answer your questions.
I am very aware of clitoral, vaginal, and cervical nerve-sparing with careful tissue dissection. However, I don’t believe most people even think about this because it’s not taught in med school or residency. Nor is there much information in general.
I do believe this is of benefit as another consideration before performing a hysterectomy. For a woman whose hysterectomy is due to carcinoma in situ (as an example), there is no other good choice but to take the cervix.
The PRP injection (O-Shot) helps a significant number of women increase sensation and intensity of orgasm. However, we cannot discount the effect of age, medical diseases, hormone status, mental status, health of the relationship, etc., which can significantly affect sensation.”
Stephanie Molden, MD: “Agree this is an understudied, under-taught, and overwhelming under-discussed topic! We are barely taught in gyne training about organs and sexual function or dysfunction at all. All of my learning on these topics has occurred from my own motivation and interest to help other women. Most research suggests (and we have been told) that hysterectomy doesn’t affect orgasm, but we have all seen the patient who feels otherwise. Leaving one’s anatomy as undistorted as possible is always preferable. If this was a man’s penis would we take the entire thing if we didn’t have to? We need more research, and I like the idea of finding out how a woman experiences orgasm beforehand. This would be a great study.”
There is value in bringing a list of questions along to every medical exam; uterine prolapse is no different. Libido and sensation intersect but are different manifestations of sexuality. Libido is desire; orgasm is the physical climax of sensation that results from stimulation. It is normal to have questions about sexual health, and it is important to ask them prior to any surgery that may impact sexual sensation or sex drive. Consider asking:
How will this surgery affect my sexual function?
Will an effort be made to avoid severing nerves?
Will sexual sensation come back if nerves are cut?
We repetitively hear knowledge is power, and truer words have never been spoken about surgery. Fear of the unknown is unsettling, anxiety-provoking, and spins patients in directions that are hardly beneficial heading into any medical procedure, much less one that impacts our most private sexual space. It is valuable to capture as much information up front as possible, to recognize what your anxieties are and express them to your surgeon for clarification, and ideally head into surgery in as calm a mind-set as possible. Some women grieve the loss of what was familiar, rather than loss of orgasm itself. It is important women take some time to recognize and acknowledge exactly what their needs are regarding surgical procedure end-result.